Value-based contracts, value-based payments, value-based purchasing or pricing or care… what’s all this value-based lingo? Well, 3 bits ago I gave you the value equation (Quality + Access / cost). Now let’s apply it. The basic premise is high quality, low cost healthcare exactly when one needs it (remember last bit?). There are 4 basic elements underscored in this new methodology to move away from pure fee-for-service payment:
a. Standardized Performance Measurement – what is measured must answer one of the 6 aspects, “Is care safe, timely, efficient, effective, equitable, and patient-centered?”;
b. Transparency & Public Reporting -measures must be converted into useful, accessible information for purchasers, payers, and consumers to inform decision making; because reporting improves outcomes (this has been clearly demonstrated);
c. Payment Innovation – re-thinks how to reimburse providers based on demonstrated performance and re-designs payment methodologies to better align economic incentives with desired outcomes. Differential reimbursement, or “pay for performance,” reflects the principles found in the rest of our economy that how much we pay for something is determined by its quality;
d. Informed Consumer Choice – encouraging and motivating consumers to change their behaviors and to choose better performance, to make choices in health and health care on the basis of value to them.
Think about these “value-based” phrases coming from the payer’s (or customer’s) perspective, in other words, government, insurance companies, employers, patients. This is what is demanded of us now in some systems and in the future uniformly. Remember, don’t kill the messenger.
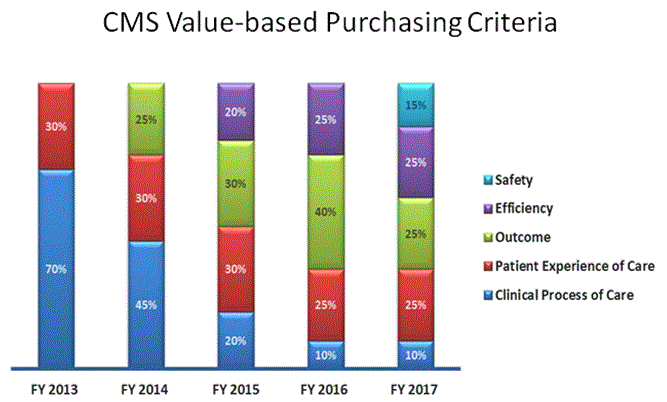
*The slide below shows you how our Medicare scores break down by weight of criteria, for hospital-based care, as new criteria are introduced each year.