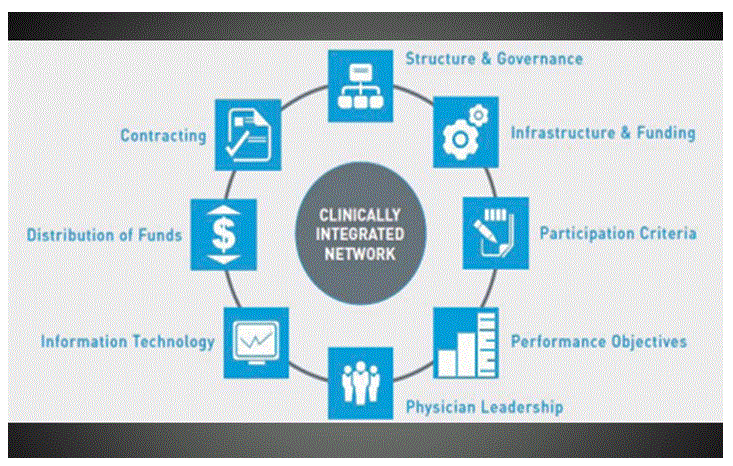
The slide from my last bit was a schematic of the 8 important components of a clinically integrated network (CIN). Here it is again below. We have covered structure & governance, infrastructure & funding, and participation criteria. And so we continue with 3 more:
A. Performance Objectives:
This is quite wide open, but the CIN must use metrics to demonstrate outcome-oriented value to the market. Typically, initiatives are chosen by the physicians but from 3 categories – clinical efficiency (reducing waste in the system), inpatient/outpatient quality (metrics appropriate to primary care specialties), and patient experience (safety and/or satisfaction).
B. Information Technology:
Obviously this is central to the CIN’s ability to measure performance and to provider’s ability to communicate with each other, and has the tools to monitor and report. The 800 pound gorilla is the interoperability of disparate systems. That’s where some capital becomes necessary, to set up a health information exchange and registries, and to purchase new tools to get the job done. But the digital heath walls that have been built to prevent encroachment by another vendor’s products are breaking down so that systems can work together as we need them to.
C. Physician Leadership:
Although a health system initiates development of a CIN, many groups that have come before us explain how critical it is to be driven by the physicians. Physicians must be engaged in the development phases, and must communicate goals and objectives clearly to peers. Physician leadership as the chair of each CIN committee, with an administrative vice-chair, has been recommended to me multiple times and written in many forms.
Next time we will finish the CIN overview with a touch of 2 complicated topics integral to the CIN structure: distribution of funds and contracting. Keep reading because I am seeing this possibly in your future!