WARNING: more acronyms in this bit but you need to know this.
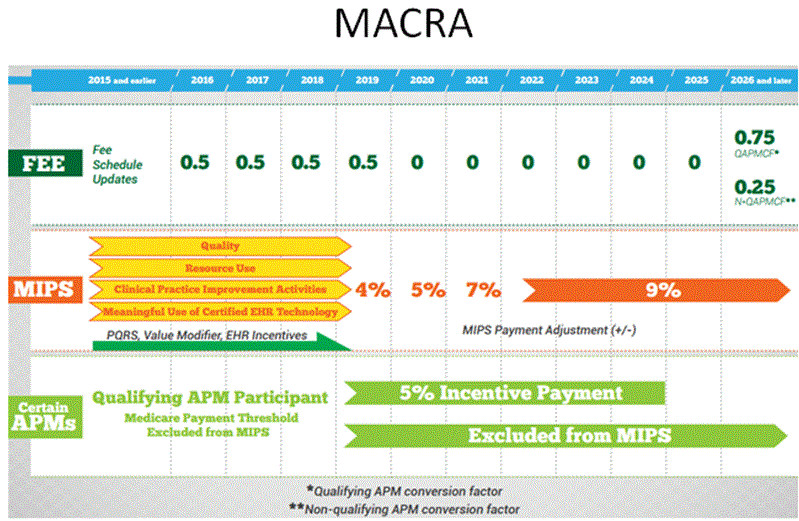
As if you haven’t had enough of these acronyms from CMS, I am introducing another one. Last year, the SGR (sustainable growth rate) formula was replaced by MACRA – Medicare Access & CHIP Reauthorization Act. The SGR formula would have cut payments to providers severely, but CMS took the opportunity to make multiple policy changes beyond just adjusting Medicare payments. The good news is that MACRA increases payment rates by 0.5% annually through 2019, instead of cutting rates. But it also consolidates and expands pay-for-performance incentives that we use now – Meaningful Use, PQRS, EHR incentive program and Physician Value-based Modifier – into a single payment adjustment to physician payments starting in 2019. This adjustment is called the Merit-based Incentive Payment System (MIPS) and includes a composite 0-100 point score. Adjustments in reimbursement will eventually range from -9% to +9%, but not until 5 years from now.
If you want, you can opt out.
Well of course there’s a catch! To opt out of MIPS, you have to participate in APMs (alternative payment models). To qualify, you must take on “more than nominal” financial risk, which is > 25% revenue in APMs in 2019, rising thereafter. Examples of APMs include bundled payments and capitated population health models. The following criteria also need to be met: using quality measures similar but not as detailed as MIPS, and using EHR technology. If we are able to successfully implement a clinically integrated network together, this APM model is unlikely to give us trouble.
Next time, we begin to dive into the rationale & structure of clinically integrated networks.