Last time, we discussed the impact of penalties now and in the future. Now we outline the complexity of measuring performance by government methodology. We have been forced to deal with a penalty system where the performance metrics as well as the type of penalty are changing yearly. In order to deal with this effectively, you need to plan ahead 2-3 years. How you are reimbursed next year depends on your performance last year – it’s already too late. And the metrics you pick to be evaluated by this year will often change next year. If that’s not enough to make you schizophrenic, try figuring out all the types of penalties: QRUR, MU, HEDIS, CQM, VBM, MIPS, GPRO, PQRS…and there will be more. Understanding all this is beyond the scope here and beyond the message of this piece: we all need a tool to aggregate clinical data, and we all need to be analyzing our data, making data-driven decisions that improve our performance and lower our costs in the future. Furthermore, we need to plan ahead, and we need to accept that commercial payers will follow suit after CMS entrenches this (private insurance will also be based on these methodologies).1
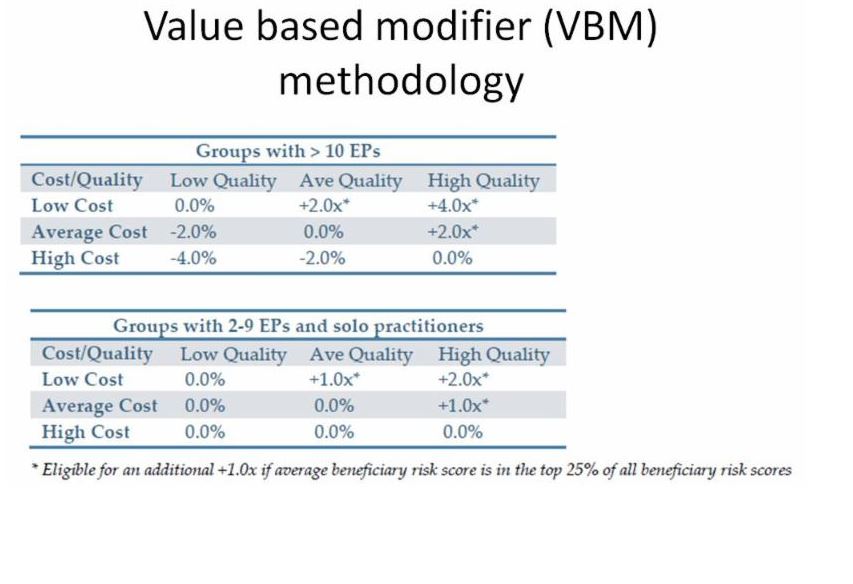
Is it all worth it? Yes, it is… first because eventually we will have no choice if we want to practice medicine, and second because for the medium term future, we are incentivized financially to perform at the top of our game. Physicians achieving high quality results at low cost will be rewarded. Small groups have less downside risk in the VBM (value-based modifier) methodology, which is one of the programs above (see table). But everyone is incentivized on the upside. The more we work towards this goal, the better we will be prepared for the alternative payment methodologies like bundled payments and population health, where we are at some degree of financial risk (remember last week’s examples?).
¹See the next bit on proof that ALL insurance payers will participate, not just Medicare.